Acute myeloid leukemia (AML) remains a therapeutic challenge with high mortality rates despite intensive and myeloablative therapies. Structural and sequence alterations have been linked to outcomes in pediatric AML and have been used for risk-based therapy allocation with modest success. Given the vast heterogeneity of AML, conventional cytogenetic and mutational (cytomolecular) biomarkers have not yielded a robust prognostic model: nearly one-third of pediatric patients deemed "low risk" relapse and, inversely, approximately one-third of those in "high risk" categories have favorable outcomes. AML studies in adults previously identified a leukemia stem cell score (LSC17) that was highly prognostic across five independent cohorts comprised of adult patients with diverse AML subtypes (n = 908). We reasoned that incorporating a similar scoring system in pediatric AML would lead to improved prognostic risk models.
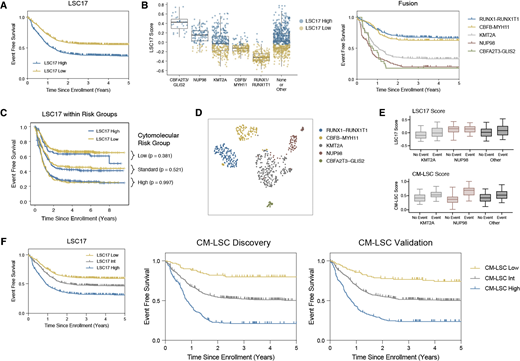
To assess for the effects of LSC17 on pediatric AML, we leveraged transcriptome sequencing data from bone marrow aspirates and peripheral blood collected from 1,503 children, adolescents, and young adults with AML at the time of diagnosis. Patients were enrolled on one of three upfront phase III Children's Oncology Group trials spanning the past three decades: CCG-2961, AAML0531, and AAML1031. In aggregate, patients with a high LSC17 score had an event free survival (EFS) of 36.9 ± 3.5% at 5 years from diagnosis compared to 55.3 ± 3.7% for those with low LSC17 scores (p < 0.0001). (Figure 1A) LSC17 scores were also associated with adverse overall survival (OS): 51.9 ± 3.9% versus 73.8 ± 3.5% (p < 0.0001) (data not shown). Intriguingly, we found that LSC17 scores significantly cluster within fusion groups and that median LSC17 scores closely correlate with survival based on fusion status (Figure 1B). Thus, when the impact of LSC17 scores was evaluated in the context of established cytomolecular risk groups, LSC17 scores were no longer predictive of outcome (Figure 1C). We then asked whether LSC gene expression data could be utilized to generate a more robust risk classification schema in the context of disease defining structural variants. Importantly, AMLs diagnosed in children, adolescents, and young adults are associated with frequent driver gene fusion alterations that also play an important role in risk stratification and transcriptional landscape (Figure 1D). We went on to confirm that AML fusion groups occupy distinct transcriptional stages of hematopoietic stem cell and myeloid progenitor maturation based on gene set enrichment analysis (GSEA) using normal hematopoiesis transcriptome experiments as their reference (data not shown).
To develop more predictive biomarkers related to stemness, we used the 54 original LSC genes identified by Ng S, et al. and performed linear regression based on a least absolute shrinkage and selection operator (LASSO) algorithm to fit a Cox regression model for patients within each fusion group. The study population was divided into discovery (n = 752) and validation (n = 752) cohorts using stratified randomization based on fusion status (RUNX1-RUNX1T1, CBFB-MYH11, KMT2A, NUP98, CBFA2T3-GLIS2, and Other/None). In the discovery cohort, we identified distinct LSC signatures that best distinguished outcome cohorts in patients with conventional high/standard risk disease (KMT2A, NUP98, and Other/None fusions) (Figure 1E). For patients deemed favorable risk (RUNX1-RUNX1T1 and CBFB-MYH11 or core binding factor/CBF), LSC signatures were not reliably predictive based on "leave one out" cross validation. Therefore, we performed multivariable analysis incorporating clinical, mutational, and transcriptional signatures to determine the factors that best discriminated outcomes with CBF AML, and found GLIS2-like transcriptional signatures were most predictive. These cytomolecular and LSC (CM-LSC) biomarkers were then combined to build a robust risk determination model that was then validated in an independent cohort (Figure 1F). This study demonstrates that a 54 LSC gene expression panel can enhance the predictive power of conventional cytomolecular markers and can more effectively partition patients into risk groups.
Cooper:Celgene: Other: Spouse was an employee of Celgene (through August 2019).
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal